Unraveling the Genetic Tapestry: Assessing Polygenic Risk in Cardiovascular Mortality
Amidst the sterile confines of a bustling hospital, a middle-aged man clenches his chest, gasping for breath. Moments later, the diagnosis of heart failure lands like a ton of bricks, revealing the silent dangers that lurk beneath the surface of his DNA. This scene echoes across the globe, as cardiovascular disease (CVD) continues to reign as a leading cause of death, accounting for approximately 30% of all fatalities worldwide. But as science delves deeper into the genetic underpinnings of these maladies, the question looms: can our heredity predispose us to an untimely demise?
The Burden of Chronic Illness
Common chronic diseases, particularly cardiovascular disorders and type 2 diabetes mellitus (T2DM), represent an escalating public health burden. Those with diabetes face a higher risk of cardiovascular mortality than their non-diabetic counterparts, a trend that intensifies with rising glycemic levels. The need for early screening and preventive strategies has never been more paramount.
The Promise of Polygenic Risk Scores
Traditional risk factors for these diseases rarely manifest in youth, complicating early identification of high-risk individuals. Here lies the potential of polygenic risk scores (PRS), a tool that leverages the power of single-nucleotide polymorphisms (SNPs) to facilitate proactive intervention. “We can now stratify individuals based on their genetic predisposition,” asserts Dr. Emily Riverton, a renowned epidemiologist. “This could revolutionize our approach to preventive healthcare.”
Despite significant advancements, most studies have focused on specific disease prediction rather than comprehensively evaluating the impact of PRS on mortality. “If we can understand how genetics intertwine with lifestyle factors, we can formulate a more holistic approach to healthcare,” adds Dr. Samuel Carter, a geneticist with extensive experience in chronic disease research.
Understanding the UK Biobank Study
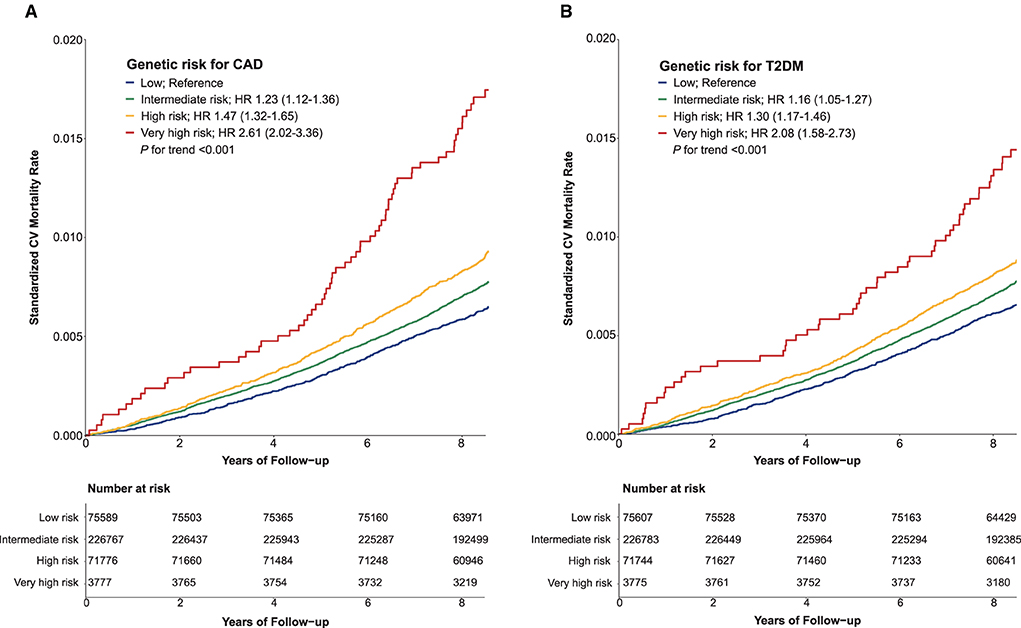
The UK Biobank, a vast repository comprising over 500,000 participants, offers fertile ground for such research. By examining a cohort of middle-aged individuals of European ancestry, recent studies sought to explore the interplay between PRS for coronary artery disease (CAD) and T2DM, lifestyle behaviors, and cardiovascular mortality.
Methodology Overview
Participants aged 40 to 69 underwent rigorous assessments, providing detailed sociodemographic information and health-related data, including lifestyle habits such as smoking and diet. The participants’ genetic profiles were established using advanced genotyping technologies, culminating in a comprehensive analysis of PRS.
- **Population**: 377,909 individuals from the UK Biobank.
- **Follow-Up**: Median duration of 8.9 years.
- **Mortality Data**: Collected from national health registries.
Findings and Their Implications
As the study unfolded, researchers discovered that a staggering 21% of deaths within the cohort were attributable to cardiovascular issues. Higher genetic risks significantly correlated with elevated cardiovascular mortality, even in individuals leading healthy lifestyles. “These findings emphasize that while genetics play a critical role, lifestyle adjustments can dramatically alter outcomes,” highlights Dr. Riverton.
Interplay of Lifestyle and Genetic Risk
Intriguingly, the study revealed that unfavorable lifestyle choices exacerbated the mortality risk associated with elevated genetic predisposition. “The combination of genetic risk and poor lifestyle choices can be catastrophic,” warns Dr. Carter. “Individuals with high genetic risks who indulged in unhealthy habits faced a compounded threat of cardiovascular mortality.”
Precision Medicine on the Horizon
The emerging data supports a predictive model for cardiovascular health. The two-fold increased risk of cardiovascular mortality in individuals with very high genetic susceptibility to CAD or T2DM signals a shift toward more personalized medical interventions. The findings bolster the argument for the adoption of polygenic risk scores in clinical practice. “The future of medicine lies in customizing care based on individual genetic profiles,” emphasizes Dr. Riverton.
Looking Ahead
As researchers continue to unravel the intricate relationship between our genetic makeup and health outcomes, the implications for public health are profound. “Implementing genetic screening could lead to significant reductions in mortality rates if coupled with effective lifestyle interventions,” suggests Dr. Carter.
The journey towards precision medicine is only just beginning. As we deepen our understanding of the multifaceted influences on health risk, society stands on the precipice of a transformative era, where each individual can be empowered to take command of their health, leaning into both their genetic insights and lifestyle choices that matter.
Source: www.frontiersin.org