Post-Acute Sequelae of COVID-19: Understanding the Long-Term Impact
In a quiet suburban home in Ohio, 38-year-old Sarah Mitchell stares blankly at the wall, grappling with a fatigue that feels insurmountable. A once-active mother of two, she now struggles to complete mundane tasks. “I feel like I’m living in a fog,” she states, her voice heavy with a mixture of frustration and confusion. This is not just a personal struggle; it is a shared experience among millions around the globe suffering from what is dubbed ‘long COVID,’ a condition emerging as one of the most significant public health challenges following the pandemic.
The Expansive Burden of Long COVID
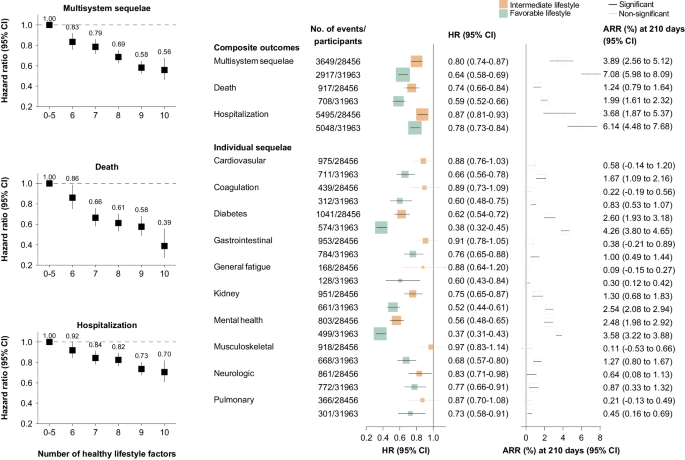
The phenomenon of ‘long COVID’ has transformed from a collection of anecdotes into a recognized clinical entity that poses profound implications for both individuals and healthcare systems. Research published in The Lancet Respiratory Medicine reveals that nearly 30% of those infected with SARS-CoV-2 will experience symptoms long after the acute infection subsides, manifesting in diverse, multisystem complications. The need to address the burden of these post-acute sequelae is urgent as affected individuals grapple with debilitating health issues.
A Vulnerable Population
Recent studies highlight that certain populations are disproportionately affected by long COVID, with patients who experienced severe cases in particular exhibiting a range of symptoms including chronic fatigue, cognitive impairment, and mental health disorders. According to Dr. Maria Santos, a pulmonologist at Boston General Hospital, “Our understanding of long COVID is evolving, but it’s clear that we are only beginning to scratch the surface of its implications. We need systematic studies to uncover the underlying mechanisms.”
- Multisystem Manifestations: Symptoms can affect numerous organ systems, including the respiratory, cardiovascular, and neurological systems.
- Psychological Impact: Emerging data indicates a significant increase in anxiety, depression, and stress-related disorders among long COVID patients.
- Healthcare Costs: The financial implications for families and healthcare systems could be staggering, with estimates suggesting billions spent on long-term caregiving and treatment.
Scientific Exploration of Long COVID
In their 2023 paper, Davis et al. explore major findings related to long COVID, emphasizing the complexity of treatment and diagnosis. The study reveals that “there are significant gaps in knowledge that hinder effective management of this condition.” Furthermore, the investigation elevates the critical need for a standardized approach to assessing long COVID, a sentiment echoed in the work conducted by Munblit et al. The Delphi consensus study outlines a core set of outcomes that should be prioritized in both clinical practice and research.
“Establishing a core outcome set for long COVID will allow us to unify our efforts in research and improve communication between caregivers and patients,” states Dr. Ellen Park, a public health researcher at the University of California, Berkeley.
Challenges in Treatment
Despite the growing awareness and burgeoning research, therapeutic avenues for long COVID suffer from a lack of evidence-backed interventions. A systematic review conducted by Tsampasian et al. indicates a desolate landscape of proven treatment options, leaving many practitioners feeling ill-equipped to support their patients. “The frustration lies in the inability to provide concrete solutions,” notes Dr. Jordan Lee, an internist at a New York City hospital. “We need to move past promising hypotheses to effective treatments.”
Patient Voices: Living with Long COVID
The voices of patients resonate deeply in this conversation. Stories like Sarah’s are filling emergency rooms and long-term care facilities with individuals who increasingly feel forgotten by a healthcare system ill-prepared for their unique challenges. Many, like Sarah, recount challenges that do not solely consist of fatigue but include pervasive brain fog and even heart palpitations.
“I was told it was ‘all in my head’—but it’s not,” Sarah asserts. “I used to run marathons, and now I can barely walk up the stairs without gasping for air. I just want to get back to my life, but it feels impossible.”
Reports indicate that younger individuals, who rarely faced serious complications during the acute phase of their illness, are now confronting an unexpected reality. According to a long-term health outcomes study conducted by Al-Aly et al., the association between mild-to-moderate COVID-19 infections and persistent health issues is alarming.
Looking Ahead
A supportive care model will be crucial in addressing the complexities of long COVID. The establishment of specialized clinics treating long COVID, alongside standardized screening processes, has begun in many countries. The implementation of new initiatives could help alleviate the burden on healthcare systems and ensure that patients like Sarah receive appropriate care.
As healthcare professionals strive to understand this condition better, the adaptation of new research findings into clinical practice will be paramount. However, the journey towards effective treatment is far from over. “We cannot afford to overlook this,” emphasizes Dr. Samantha Groves, a researcher and long COVID advocate. “The long-term health landscape following COVID-19 must include these voices for change.”
As societies continue to grapple with the aftermath of the pandemic, the enduring ramifications of long COVID stand as a stark reminder of the virus’s reach. It urges a collective conversation about individuality and community health, encapsulating the dual reality, where recovering from COVID-19 is only the beginning of a new struggle for many.
Source: www.nature.com